- +1 800 433 4609
- |
- Request Info
- |
- Login
Event-related potentials (ERPs)
Event-related electroencephalography (EEG) is an advanced method that allows researchers and clinicians to observe how the brain responds specifically to external stimuli, such as visual or auditory signals. The goal is to measure and isolate brain activity responses directly related to the presented stimulus, providing precise insights into cognitive processes.

How Does Event-Related EEG Work?
Baseline Brain Activity vs. Stimulus Response: At rest, your brain performs continuous EEG activity, consider it the background noise activity reflecting your ongoing mental state and internal thoughts. When a stimulus is presented, it triggers distinct brain responses. The challenge is isolating these stimulus-specific responses from the ongoing, unrelated EEG background activity.
Stimulus-Triggered Activity: When a sensory stimulus (visual or auditory) is introduced, the brain generates a specific electrical response known as an Event-Related Potential (ERP). For example, viewing an image or hearing a sound will elicit unique EEG patterns (from each electrode) directly linked to processing that stimulus.
Multiple Trials for Accuracy: Stimuli are briefly presented multiple times (usually 30 or more trials). EEG data are recorded and segmented around each stimulus (epoch), typically ranging from 200ms before to 1000ms after stimulus presentation.
Data Averaging Technique: After removing trials affected by artifacts (such as eye movements or muscle activity), the remaining EEG segments are averaged across trials. Through averaging, unrelated background activity ("noise") is reduced, leaving clearer and more precise stimulus-related EEG response patterns.
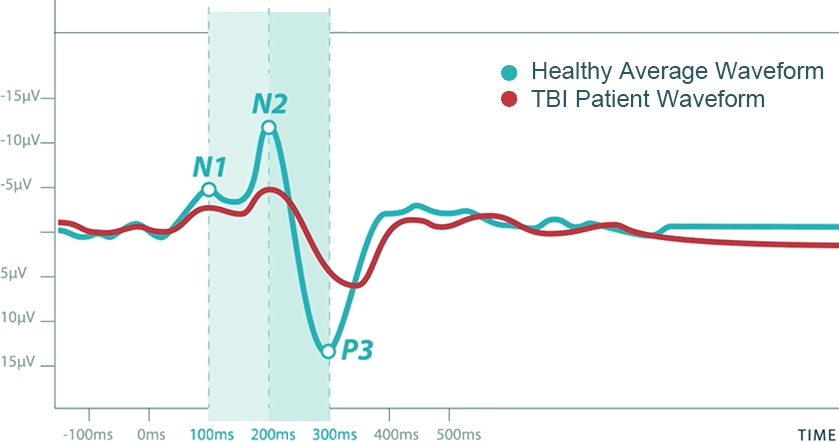
Resulting Data: The averaged EEG segments result in a clear waveform, known as an event-related potential (ERP). ERP response waveforms reflect distinct cognitive processes, with each component identified by its shape, latency (time), amplitude (strength), and scalp topography (the pattern of activity across electrodes).
Baseline Brain Activity vs. Stimulus Response: At rest, your brain performs continuous EEG activity, consider it the background noise activity reflecting your ongoing mental state and internal thoughts. When a stimulus is presented, it triggers distinct brain responses. The challenge is isolating these stimulus-specific responses from the ongoing, unrelated EEG background activity.
Stimulus-Triggered Activity: When a sensory stimulus (visual or auditory) is introduced, the brain generates a specific electrical response known as an Event-Related Potential (ERP). For example, viewing an image or hearing a sound will elicit unique EEG patterns (from each electrode) directly linked to processing that stimulus.
Multiple Trials for Accuracy: Stimuli are briefly presented multiple times (usually 30 or more trials). EEG data are recorded and segmented around each stimulus (epoch), typically ranging from 200ms before to 1000ms after stimulus presentation.
Data Averaging Technique: After removing trials affected by artifacts (such as eye movements or muscle activity), the remaining EEG segments are averaged across trials. Through averaging, unrelated background activity ("noise") is reduced, leaving clearer and more precise stimulus-related EEG response patterns.
Resulting Data: The averaged EEG segments result in a clear waveform, known as an event-related potential (ERP). ERP response waveforms reflect distinct cognitive processes, with each component identified by its shape, latency (time), amplitude (strength), and scalp topography (the pattern of activity across electrodes).
Characteristics of Event-Related Potentials (ERPs)
ERPs can be described using several key characteristics:
ERPs can be described using several key characteristics:
- Shape and appearance - The overall waveform pattern.
- Number and timing of components - Positive and negative peaks in the signal.
- Latency - The time at which different components appear relative to stimulus onset.
- Amplitude - The strength of the response at specific time points.
- Topography - The spatial distribution of voltages across different EEG electrodes.
Some of the most well-researched ERP components include:
- N200 - Involved in facial recognition and early visual processing.
- P300 - Associated with attention and stimulus evaluation.
- N400 - Related to semantic processing and language comprehension.
Clinical and Research Applications of ERPs
ERPs help identify and analyze cognitive processing differences across conditions or populations.
Scientists often compare ERPs under different experimental conditions, such as:
- Face stimuli vs. house stimuli - To study visual processing differences.
- Children with Autism Spectrum Disorder (ASD) vs. age-matched neurotypical controls - To examine neurodevelopmental differences.
Comparisons typically focus on ERP latency, amplitude, or topographic differences between conditions or participant groups. By analyzing these variations, researchers gain deeper insights into cognitive processing, perception, and neurological disorders.
What is an ERP Analysis?
Event-related potentials (ERP) are also called evoked potentials (EP) and measure the brain's direct response to a specific sensory, cognitive, or motor event. EPRs can measure (to the millisecond) the brain's speed to process this information. This fast-paced processing allows us as humans to receive, filter, and process billions of pieces of information to make split-second decisions every second of every day. Due to the sensitivity of ERP testing, we can detect changes in this processing speed related to cognitive decline. Performing testing early on can show changes before becoming physically noticeable. As a result, the ERP can detect slowing in physical reaction times, decision-making skills, stress disorders, memory loss, and other neurological disorders.
An Event-Related Potential (ERP) is an electrical potential detected by Electroencephalography (EEG) used to understand how the brain processes visual and auditory information. It occurs after a sensory stimulus occurs. ERPs are measured while a patient is engaged in a task. It is an added tool used and often offers more detail than the standard detailed neurological examination.
Memory functions and cognitive processes within the brain can be measured using event-related potentials (ERPs). The latency or time delay between the onset of the stimulus and a patient's physical response reflects brain processing speed. In contrast, waveform amplitude reflects neuronal recruitment and subsequent activation of the recruited neurons to process the information.
Fundamental ERP elements include the degree of attention to stimulus and the subsequent encoding of information for storage and retrieval. P300a and P300b are two ERP components useful in measuring these aspects of memory and brain activity. The P300b component has been exceptionally well-studied regarding memory loss disorders, such as Mild Cognitive Impairment (MCI) and Alzheimer's disease (AD). When comparing AD to age-matched controls, AD patients had longer P300b latency measures and low amplitudes. P300b latency and amplitude can predict the progression of mild cognitive impairment. Additionally, P300b metrics demonstrate superior sensitivity over conventional assessments, such as the MMSE, detecting early preclinical memory loss.
ERP helps understand how the brain processes information and how long it takes to respond to sensory stimuli. Using ERP analysis, we better understand how the brain is processing while a patient is performing activities of daily living.
Fundamental ERP elements include the degree of attention to stimulus and the subsequent encoding of information for storage and retrieval. P300a and P300b are two ERP components useful in measuring these aspects of memory and brain activity. The P300b component has been exceptionally well-studied regarding memory loss disorders, such as Mild Cognitive Impairment (MCI) and Alzheimer's disease (AD). When comparing AD to age-matched controls, AD patients had longer P300b latency measures and low amplitudes. P300b latency and amplitude can predict the progression of mild cognitive impairment. Additionally, P300b metrics demonstrate superior sensitivity over conventional assessments, such as the MMSE, detecting early preclinical memory loss.
ERP helps understand how the brain processes information and how long it takes to respond to sensory stimuli. Using ERP analysis, we better understand how the brain is processing while a patient is performing activities of daily living.